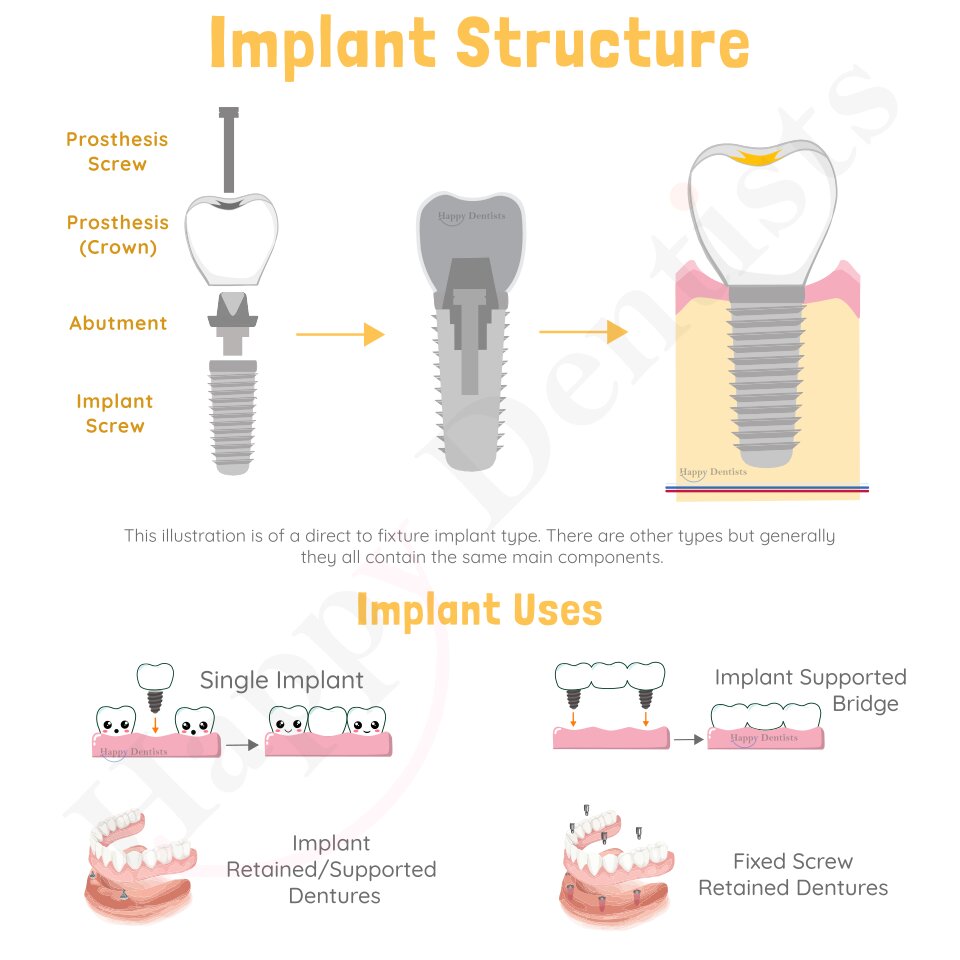
Dental implants are artificial tooth roots used to replace missing teeth.
So when people say they want a single dental implant, they usually mean they want an implant, abutment and crown. Implants and their crowns can closely resemble and function like natural teeth. As a result, dental implants have become an important part of dentistry. They are used to replace one missing tooth, several missing teeth or even a full jaw with no teeth. There are many designs and techniques available. Your oral health practitioner can help guide you on which option is best for your situation.
Learn more about dental implants below:
- Structure of an Implant
- Types of Implants
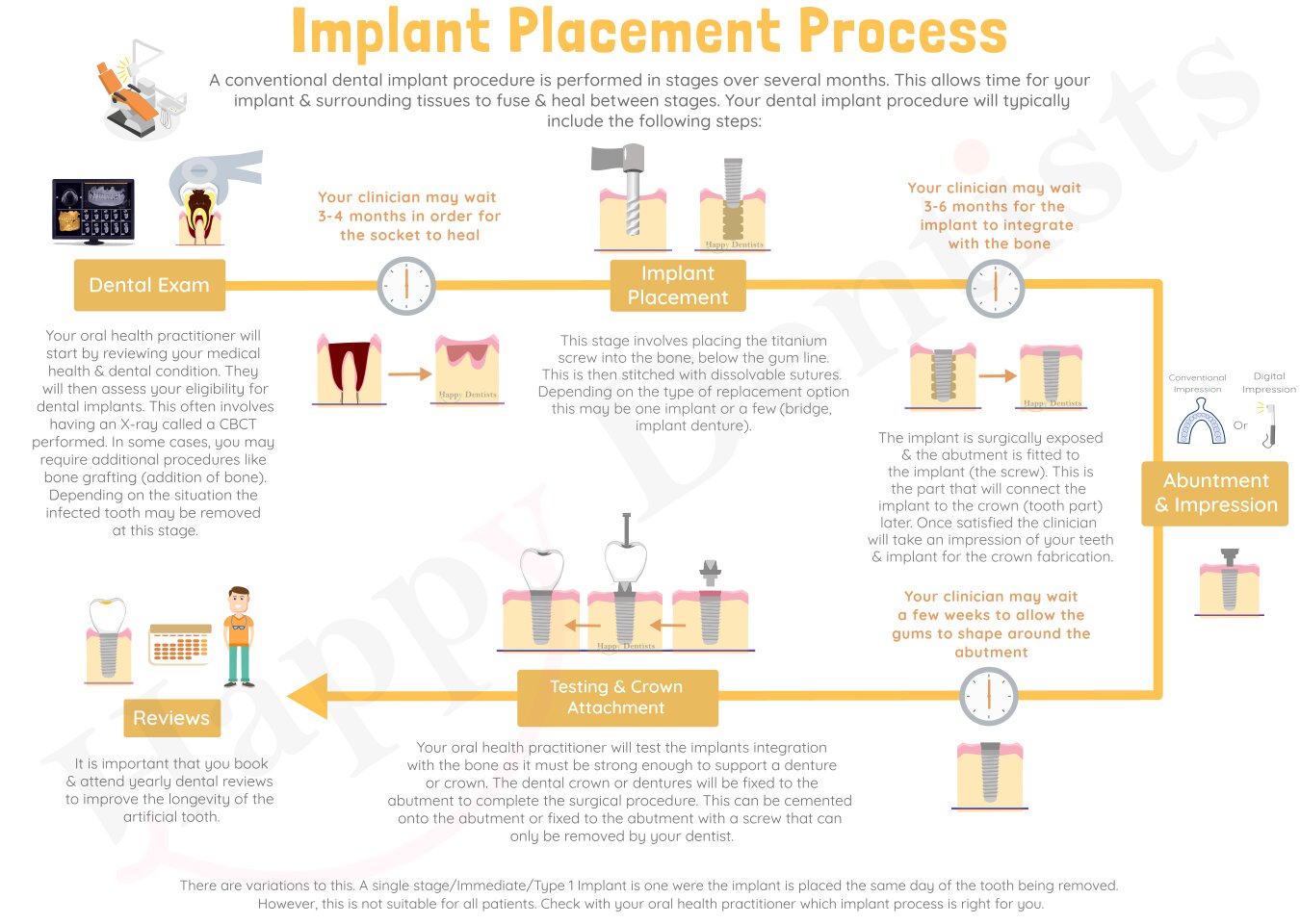
- The Implant Placement Process
- Complications
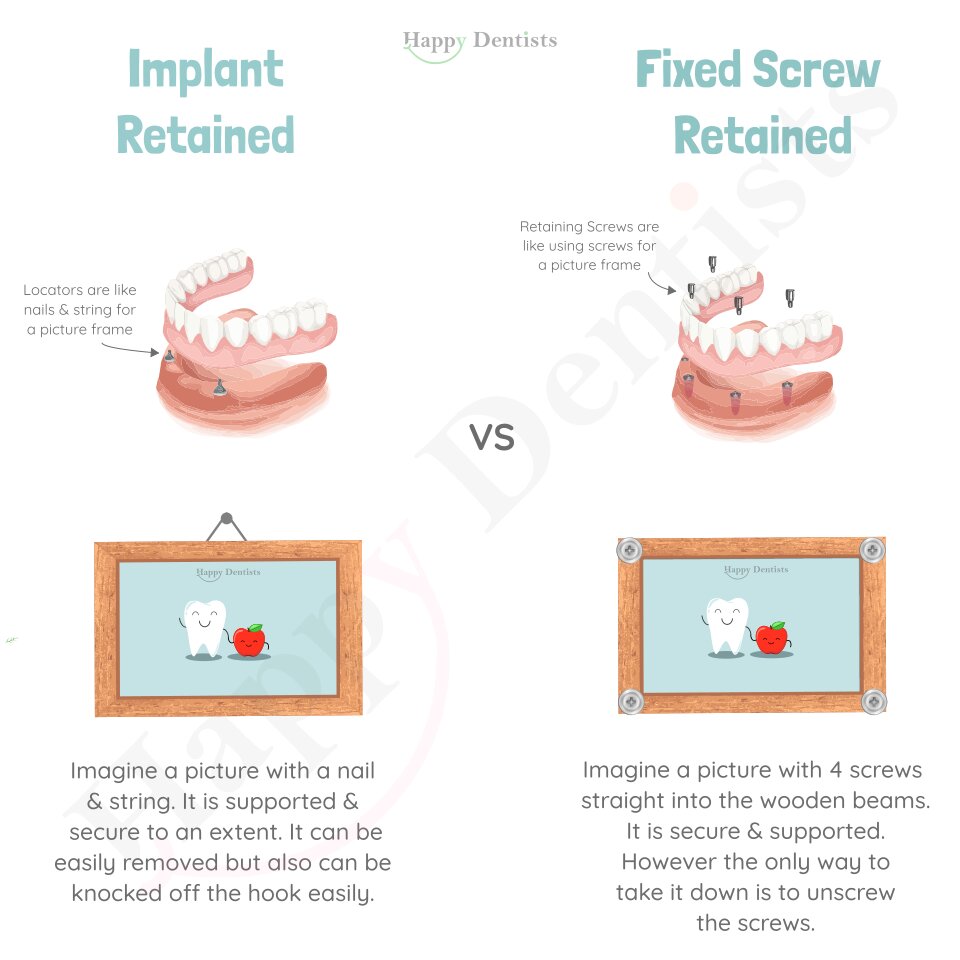
- Difference between implant retained/supported dentures and fixed screw retained dentures
- Why are dental implants useful?
- Why might I need to have fillings and a clean before getting the implant?
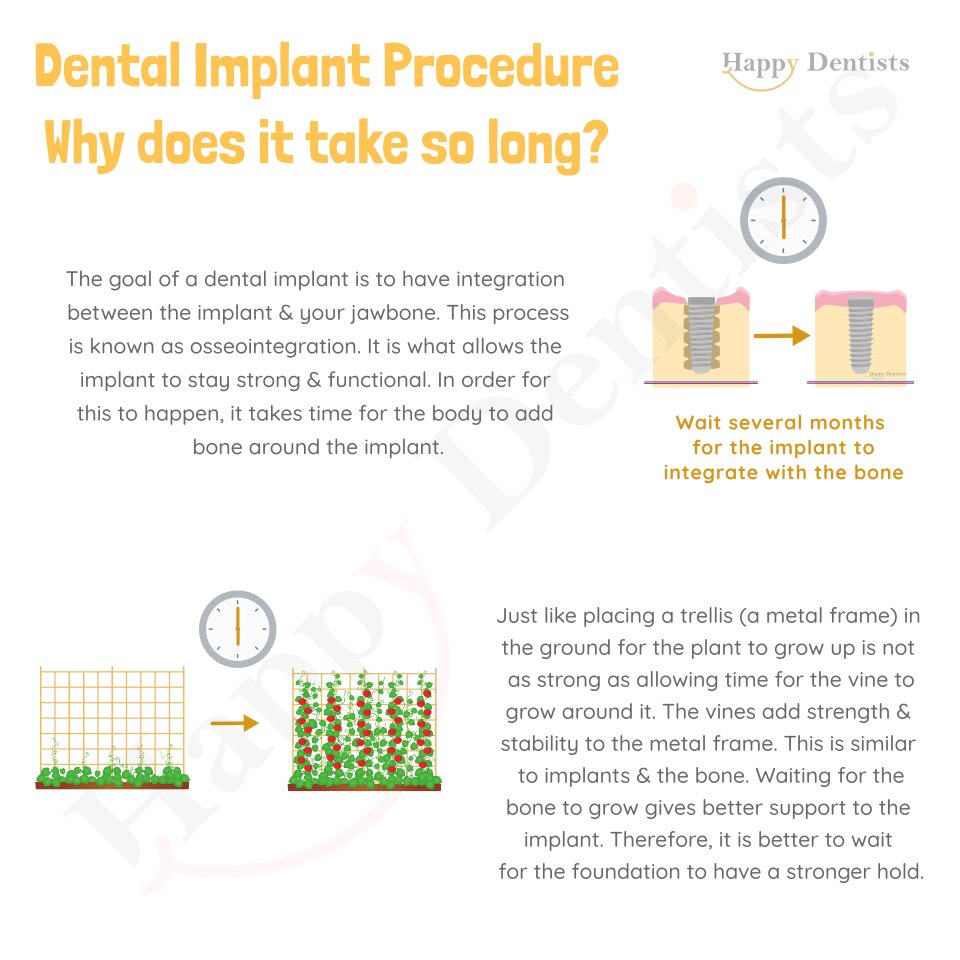
- Why does the implant process take so long?
- Is a dental implant going to be exactly like my previous tooth?
- Why does my dentist need to know my medical history and current medications before implant surgery?
- Medications (drugs):
- Conditions:
- In what situations may implant therapy not be suitable for me?
- Poor oral hygiene – due to inability or motivation. This can lead to implant failure after placement. As a result, the oral health practitioner may want to address this first.
- Bone availability in the jaw – Bone resorption occurs once the tooth has been removed. This bone loss is most rapid in the first 3 months after a tooth is extracted. It continues at a slightly slower rate in the year after the tooth is lost. After this, the bone continues to shrink but at a slow rate. In some patients they may not have adequate bone for an implant as a result. It is difficult to place an implant if there is no foundation, it is like trying a post in the ground with no cement. In these situations, you may be able to have bone replacement (bone grafting) to rebuild the site so there is sufficient bone for the implant to be placed.
- Age- Implants are teeth that are fused to the bone, they do not grow as the bone grows like the other teeth. As a result, it is often advised that people wait until early 20s before getting implants. To avoid this complication of having one tooth shorter than the others.
- Smoking – It is a good time to quit, as smoking can lead to the failure of the implant to integrate with the jawbone. Therefore, to improve the success of your implant it is advised that you stop smoking.
- Certain medications – Like bisphosphonates. This medication works by decreasing the bone turnover decreasing bone growth. Which may be a problem when we want the implant to integrate with growing bone. Thus, it can lead to failure of the implant to integrate. The risk varies with implant survival rates ranged between 95% and 100% in case of bisphosphonate users and 96.5% to 99.2% in non-users. It is important to note that oral bisphosphonates (tablet) rate is lower than intravenous bisphosphonates (injected).
- Particular medical conditions – Conditions such as uncontrolled diabetes can lead to increase risk of complications like delayed healing, infection, and peri-implantitis.
- Unrealistic expectation – a dental implant is manmade and unfortunate they are good but not that at the level to fully replicate nature. As a result, a realistic outlook is important. Sadly, it is not successful for everyone. This procedure is difficult and patient situations can add to the complexity of the procedure. Therefore, results may not be to the level that the patient had expected. As a result, it is important you have detailed discussion with your oral health practitioner to see if this option is for you.
- Psychological Conditions – the concern with the implant option for these disorders is that the patient may not be able to follow the oral health practitioner’s instructions.
- Alcohol and drug abuse/dependency – These substances may affect the patient’s ability to follow the oral health practitioner’s advice, their ability to care for the implant and maintain oral hygiene. It may interfere with good nutrition, impair healing, and affect osseointegration.
- Pregnancy – the oral health practitioner may defer treatment as general anaesthesia (if required) and other medications may place unnecessary risk on the mother and baby in some cases.
- Does having an artificial tooth mean I will not have dental problems like decay and gum disease?
- What care should I follow after my implant surgery?
- What are the four types of implant insertion timings (i.e what is are immediate, immediate delayed and delayed implants?
- Which implant insertion time is better?
- What happens if I have a tooth out and leave it for more than 6 months before getting an implant?
- What is a bone graft?
- What is the success rate of implants?
- What is the difference between implant retained/supported dentures and fixed screw retained dentures?
- How do I care for my dental implant long term?
Frequently asked questions:
Implants offer and alterative replacement option for missing teeth when traditional dentures and bridges may be more destructive and less ideal for your situation. Often people describe dental implants are more convenient, attractive, functional, and comfortable than dentures. As they feel there biting and chewing is relatively similar to normal teeth. Unlike conventional dental bridges this replacement option does not require reshaping and removing healthy tooth structure of neighbouring teeth. They can help reduce the bone loss in the jaw. They can help prevent teeth movement of neighbouring teeth as well as averting collapsed cheeks.
Dental problems need to be addressed before implant placement. This is because implants are a big procedure and you want them to be successful. However, it is not great to have one good artificial tooth when your other teeth surrounding this tooth is falling apart or disease occurring. In terms of active gum disease this has been showed to affect the longevity of the implant. This putting out small fires when they arise is not great for long term management and getting the most out of your teeth and smile. It is better to identify any problems before they become fires and then control these or remove them so they can be incorporated into a better design for the future that will last longer. For example, if you have bruxism (grinding) it is better to know this before implant placement so the oral health practitioner can design the implant to accommodate this, or supply you with a personalised mouth guard (splint). This type of treatment planning is better for your overall care and the longevity of the implant
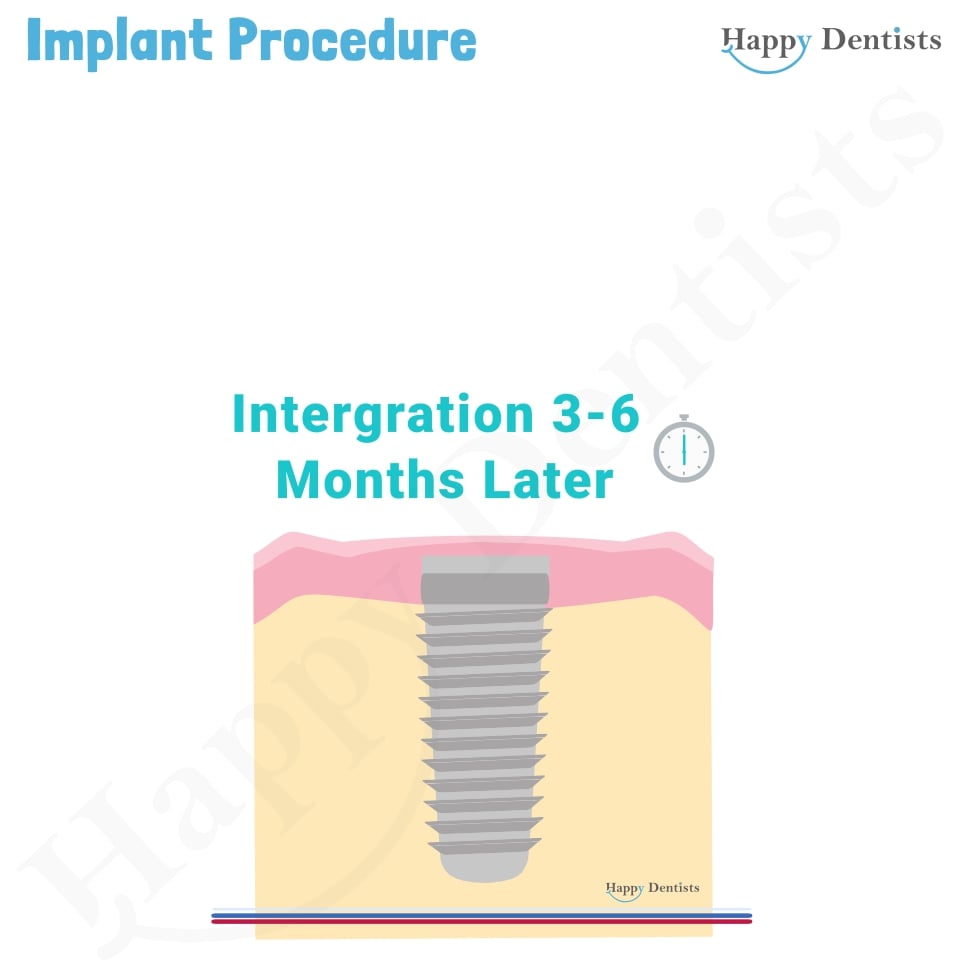
The goal of a dental implant is to have integration between the implant & your jawbone. This process is known as osseointegration. It is what allows the implant to stay strong & functional. In order for this to happen, it takes time for the body to add bone around the implant. Just like placing a trellis (a metal frame) in the ground for the plant to grow up is not as strong as allowing time for the vine to grow around it. The vines add strength & stability to the metal frame. This is similar to implants &the bone. Waiting for the bone to grow gives better support to the implant. Therefore, it is better to wait for the foundation to have a stronger hold(click here to see the picture above)
The short answer is no, not exactly. Both the function and appearance will be different to your natural teeth and it may take time to get used to this. It is a made device that is trying to replicate a biological masterpiece that has taken billions of years to develop. Your oral health practitioner will try their best to produce results that are like the natural teeth. However, the outcome is heavily dependent on the case. Some crowns and implants can be difficult because of the location of the implant placement, the bite force applied, your health, your commitment to oral hygiene, and the amount of bone. These are a few factors influencing whether not the outcome is less than you the imagined. As a result, it is important you express your concerns and expectations with your oral health practitioner so that can clarify and provide a realistic understanding of the limitations and benefits of this procedure.
This is because the success of the procedure and recovery after dental implant placement can be affected by the medications and conditions that you may have. Therefore, tell the dentist all your medications that you take every day, month, and year as well as any conditions that you have been diagnosed with. In particular for implants, it is especially important you inform your oral health practitioner if you are taking the following medications or have the follow conditions:
Medications that affect the Bone (bisphosphonates, denosumab (Prolia)).
Blood thinning medications such as aspirin, warfarin, heparin, dabigatran, or any other types.
If you are a smoker.
Have Diabetes either type 1 or type 2
Have had Facial radiotherapy
Have Haemophilia or any other kind of blood condition
Have suffered heavy bleeding following surgery or bruising after an injury
Have had Rheumatic Fever
Have had Heart surgery or any Heart problems
Have had an allergic reaction to antibiotics, anaesthetic drugs, pain killers or any other medication
If you have been diagnosed with Osteoporosis and taking any medication related to this.
Have had any condition involving long term treatment with steroids
If you been diagnosed with Gum Disease (Periodontitis)
If you are pregnant
This depends heavily on the risk that the oral health practitioner and yourself as the patient are willing to take on. As most of these increase the risk of the implant failing. As a result, some people may be advised to avoid or delay having implants for the following reasons.
No, in fact it is more likely to be the opposite. As it is an artificial tooth it no longer has a pulp which is the nerve and blood supply of the tooth nor does it have periodontal ligaments (which are like the shock absorbers of the tooth). These both usually communicate with the brain to alert you something is wrong or be careful if you do that you might break something. As a result, you must be extra careful and diligent with cleaning. Peri-implantitis (which is gum disease of the implant) is one of the main reasons why implants fail. Implants must be cleaned every day, so they stay free of dental plaque. Regular check-ups and maintenance with your oral health practitioner will help improve the chances of success and longevity. If you are unable to continue rigorous cleaning, inform your oral health practitioner as they can help to guide you with options to make this easier.
Care should be like what is done after a tooth extraction. Therefore, you may find it easier to follow the same instructions. Patients should avoid strenuous activity, rest at home, consume soft foods, and they should do not have alcohol especially while taking medications. (click here to see post extraction instructions)
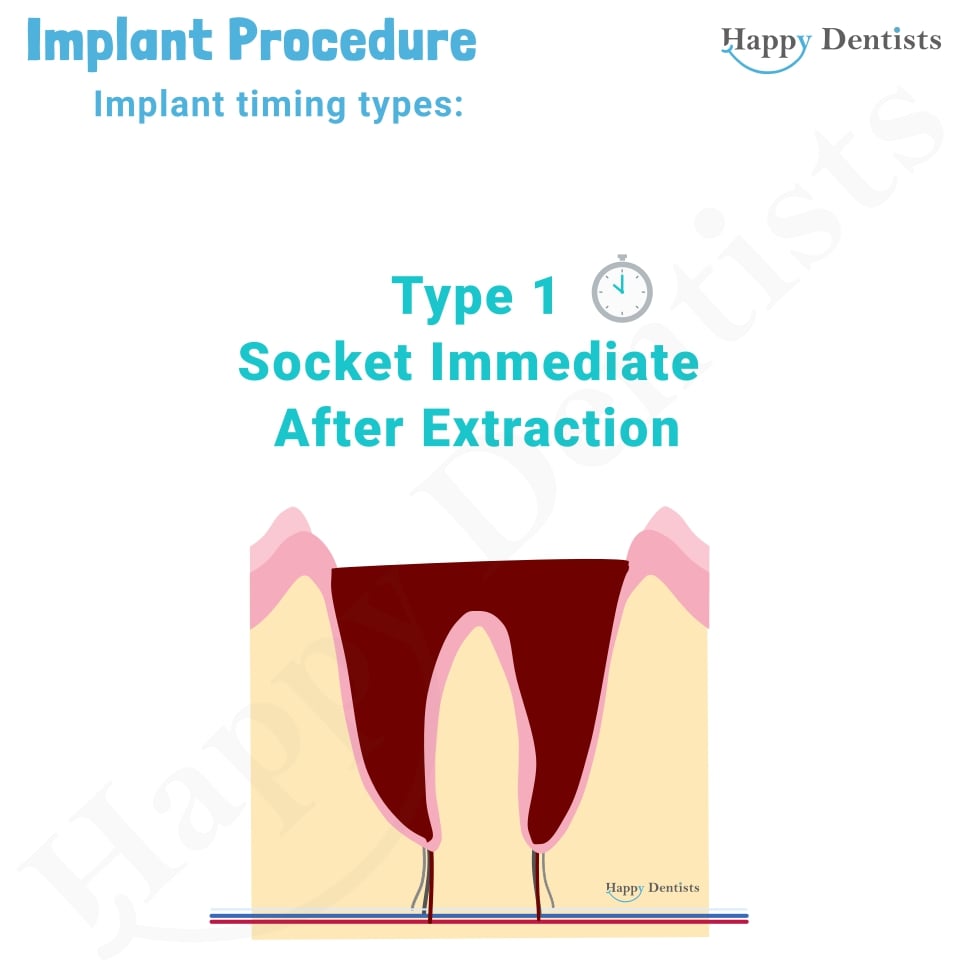
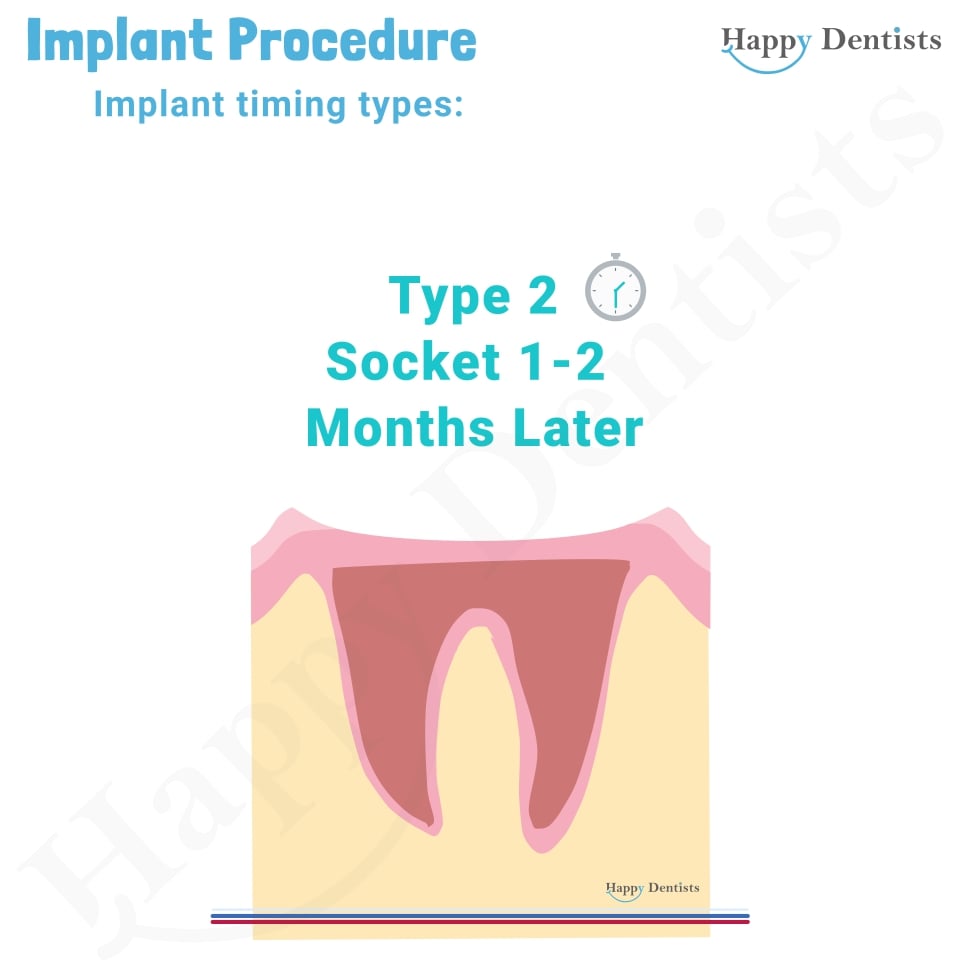
Type 1 timing is an immediate implant. This means that as soon as the tooth is taken out the implant is then placed. Remember this is the implant screw placement, it does not always mean that the crown prosthesis placed at the same time sometimes it does. But both cases are case selective. You must have certain characteristics and factors for this option to be viable to get an optimal outcome. Do not worry your local oral health practitioner will help assess if this is a viable option for you. This method does reduce the number of surgical procedures and overall treatment timeframe. However, the downside is that the bone has not had time to heal so the placement on the implant may not be in the ideal position. There is potential to have bone loss and gum loss on the lip side which will affect aesthetics. Furthermore, primary stability (which is the mechanical engagement of the implant with the bone) may be compromised. Type 2 timing is immediate delayed implants. This means that you wait 6-8 weeks after the tooth is removed before the implant process commences. This allows the soft tissue (gums) time to heal. Type 3 timing is delayed implants which means that you wait 3-4 months after the tooth is removed before the implant process commences. This allows the soft tissue (gums) and most of the bone to heal. This tends to be used by oral health practitioners as it allows better bone support, has lower risk, and is more precise. It does take more clinical sessions. Type 4 timing is when you wait more than 4 weeks after tooth removal before the implant process commences. This allows more time for soft tissue and bone healing, however, has the downside of bone loss starting to occur. More bone loss is possible the longer there is not an implant in the site. This may require additional procedures like bone lifts later. However, bone lifts are not always possible or guaranteed to work.
The literature is still researching and developing which technique is the best as all of them have their own advantages and disadvantages. At current there is no standard one method that is superior for every case. The method used will be depended on lots of factors. Some of these factors are based on your medical conditions, the situation of your mouth, the available bone support, and gums.
There is loss of bone and soft tissue overtime. If you leave it too long before having an implant placed, you may require additional procedures to try and resolve this. Sometimes these additional procedures may not be possible or may not work as they are case dependent. As a result, it is very important you inform your oral health practitioner of your future teeth replacement choice before removal of teeth so that they can help you plan for this.
This is a surgical procedure aimed at replacing missing bone. It is useful if the bone in your jaw is too soft or thin. This could have happened for many reasons, including tooth loss, injury, gum disease and infections. Talk to oral heal practitioner if this is required for your situation.
95% success rate that means that about 95 patients in every 100 can expect to have successful treatment. However, the short and long term success of the implants depend on many factors, including the health and capacity of the jaw bone to heal, the type of implant, the technique used, the number of implants placed and the type of prosthesis (Denture, bridge or crown), whether the implant is being placed on the top or bottom jaw and the general health of the patient. Unfortunately, we do not have a glass ball to determine how long the implant will last. On average they last 10 years, however, who is to say that you are the average number you may be less, or you may be more than 10 years. In some people every implant will be successful, while in others the implants may fail to integrate with the bone. Therefore, while they are not successful for everyone, they are effective for most people. Your oral health practitioner after examining you and reviewing your case will be able to provide you with a more detailed answer on the long-term success of your possible implant.
An implant retained/supported denture is a denture that is braced by a few implants. It can be removed easily to clean and is not fully fixed in. It can be removed at home to be cleaned. This is like a picture with a nail & string. It is supported & secure to an extent. It can be easily removed but also can be knocked off the hook easily. Whereas fixed screw retained denture, is a denture that has been screwed to the implants in the bone in the dental clinic. It can not be removed at home. This is like a picture with 4 screws straight into the wooden beams. It is secure & supported. However, the only way to take it down is to unscrew the screws. (click here to see the picture above)
Care should be similar to the recommended care for your teeth everyday as plaque (collection of bacteria) can adhere to the implant and lead to infection also. In fact, poor oral hygiene can shorten its lifespan, as a result good oral hygiene is crucial. Therefore, brush twice a day, use fluoride toothpaste to reduce risk of decay of your natural teeth. Use interdental brushes and a small headed toothbrush with soft bristles. Flossing is important especially for dental implants as the toothbrush does not fit under the bridge or under the gums. Tape is a good floss tape for implants. Avoid smoking as this can impair healing and increase the chance of implant failure. Sugary foods encourage decay causing bacteria build up, therefore these should be limited.
- 1. Dental examination – stage 1 Planning and Extraction. (This may be over multiple visits)
- 2. Implant placement (Preparation and insertion of the implant)
- 3. Abutment placement and impressions
- 4. Testing and Crown attachment
- 5. Follow up (Review)
- Please note there are variations to this, a single stage procedure/immediate implant/type 1 implant has the implant placed the same day of extraction. However, this is not suitable for all patients. Check with your oral health practitioner which implant
- Please note that it is not always necessary to replace every tooth with an implant in cases for a supported denture or for a bridge supported implant system.
Treatment:
See the animation belowWith a conventional dental implant, the implant procedure is performed in stages over several months. This allows time for your implant and surrounding tissues to fuse and heal between stages. Your dental implant procedure will typically include the following steps:
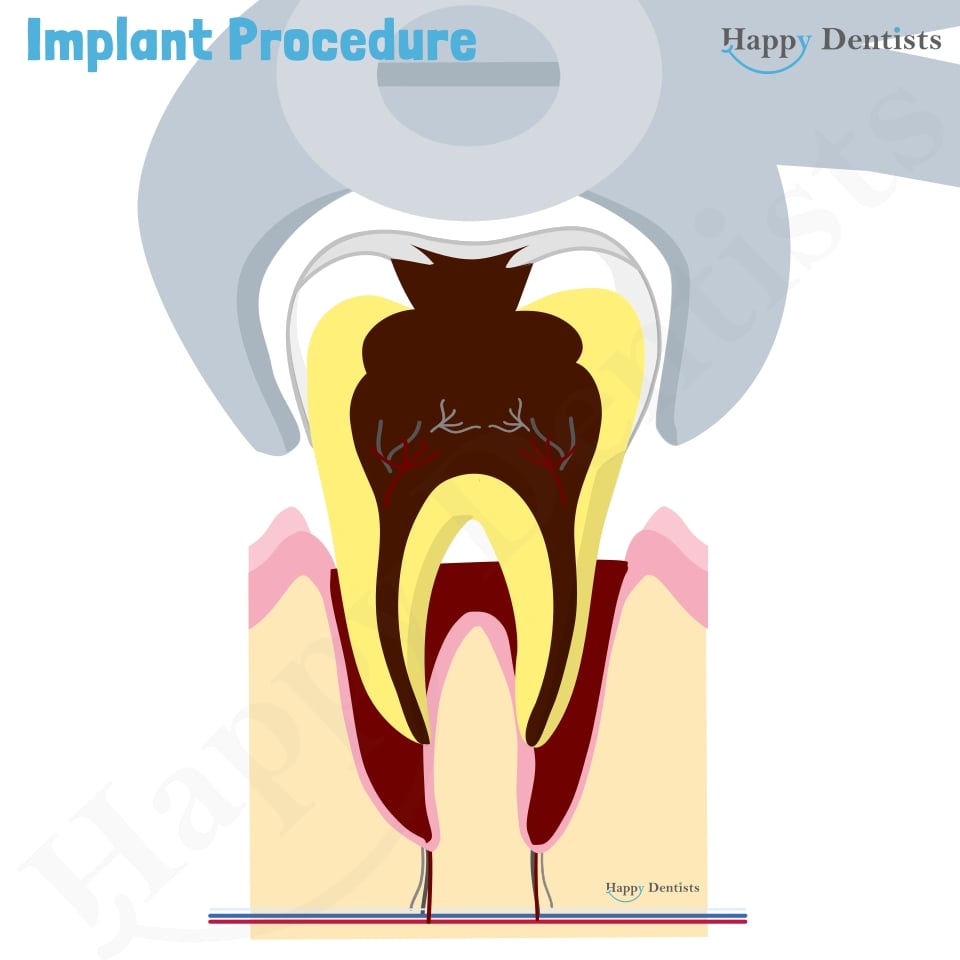
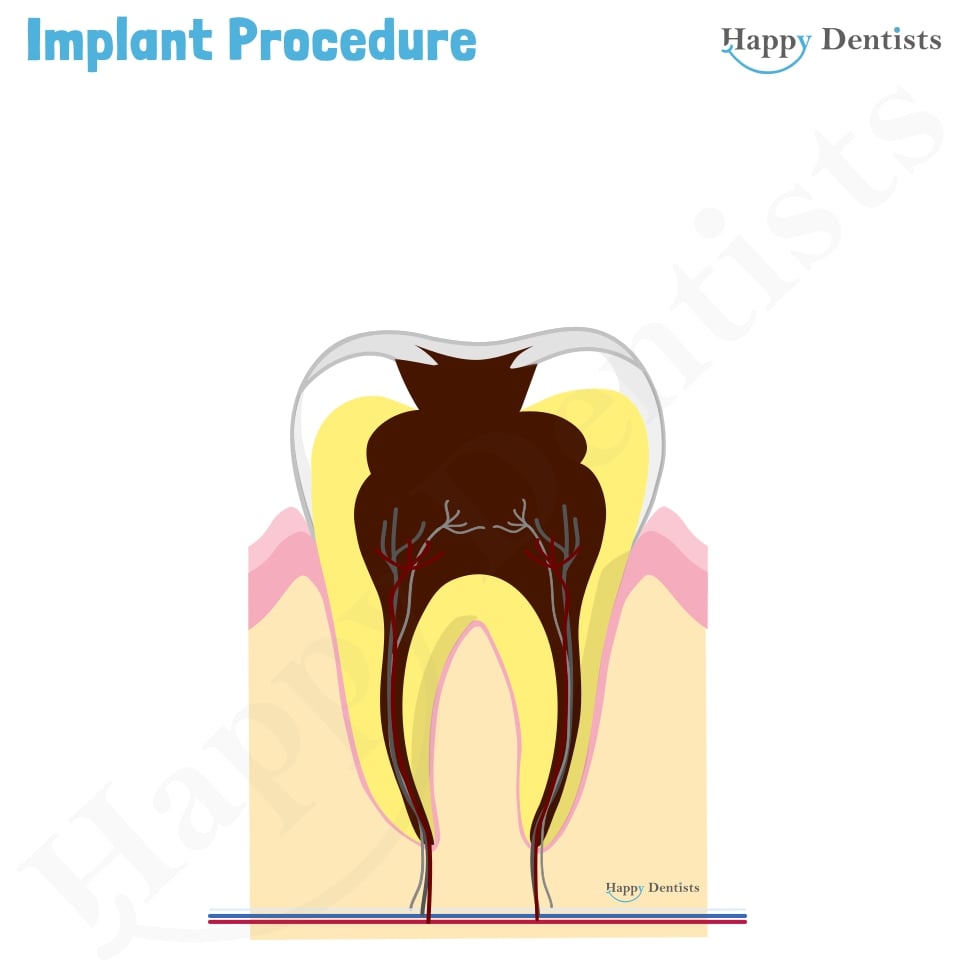
Your oral health practitioner will begin by reviewing your medical health and checking your dental condition. They will examine elements such as your bone density and gum health to determine your eligibility for dental implants. This involves having an X-ray called a CBCT performed. Before your dental implant procedure, your dentist will need to prepare the bone and surrounding area for implant surgery. In some cases, you may be required to undergo additional procedures such as bone grafting (additional for bone) if you have inadequate bone. In other cases, if the tooth is still present and it is no longer viable for it to remain in the jawbone because of decay or a fracture this will then be removed. Depending on the technique, clinician may wait to allow the jawbone to heal.
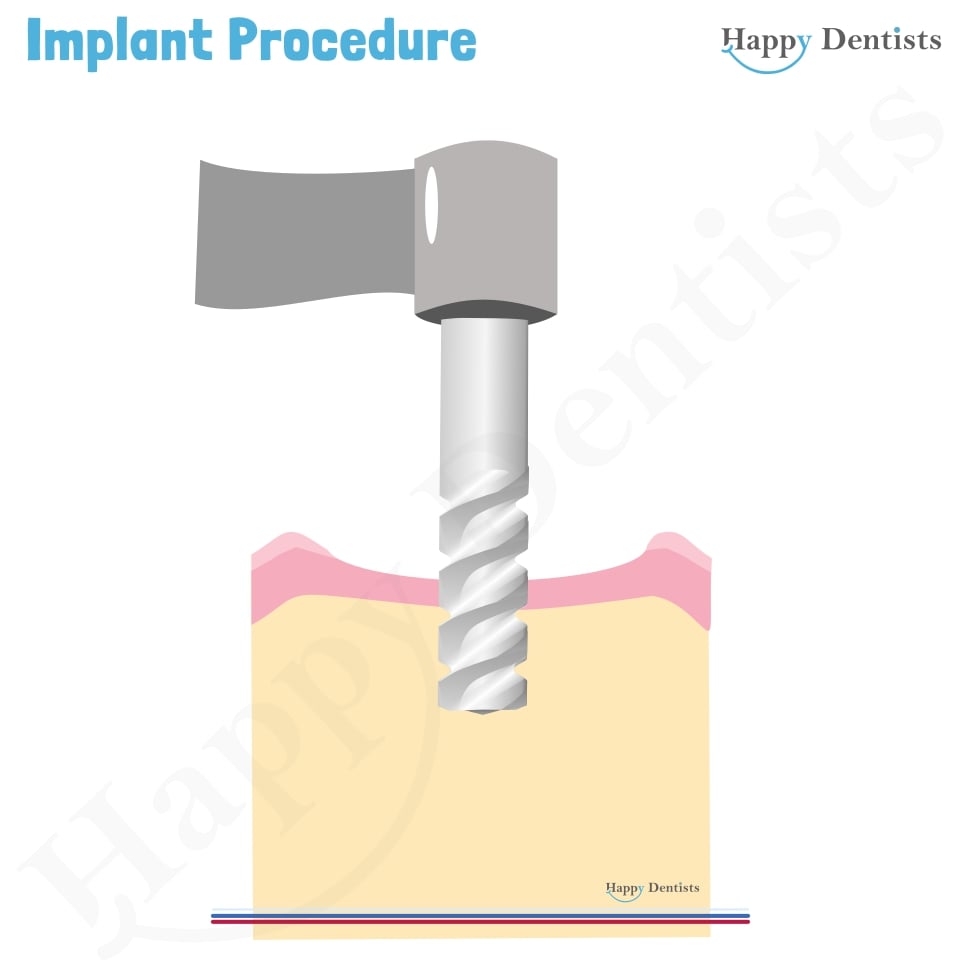
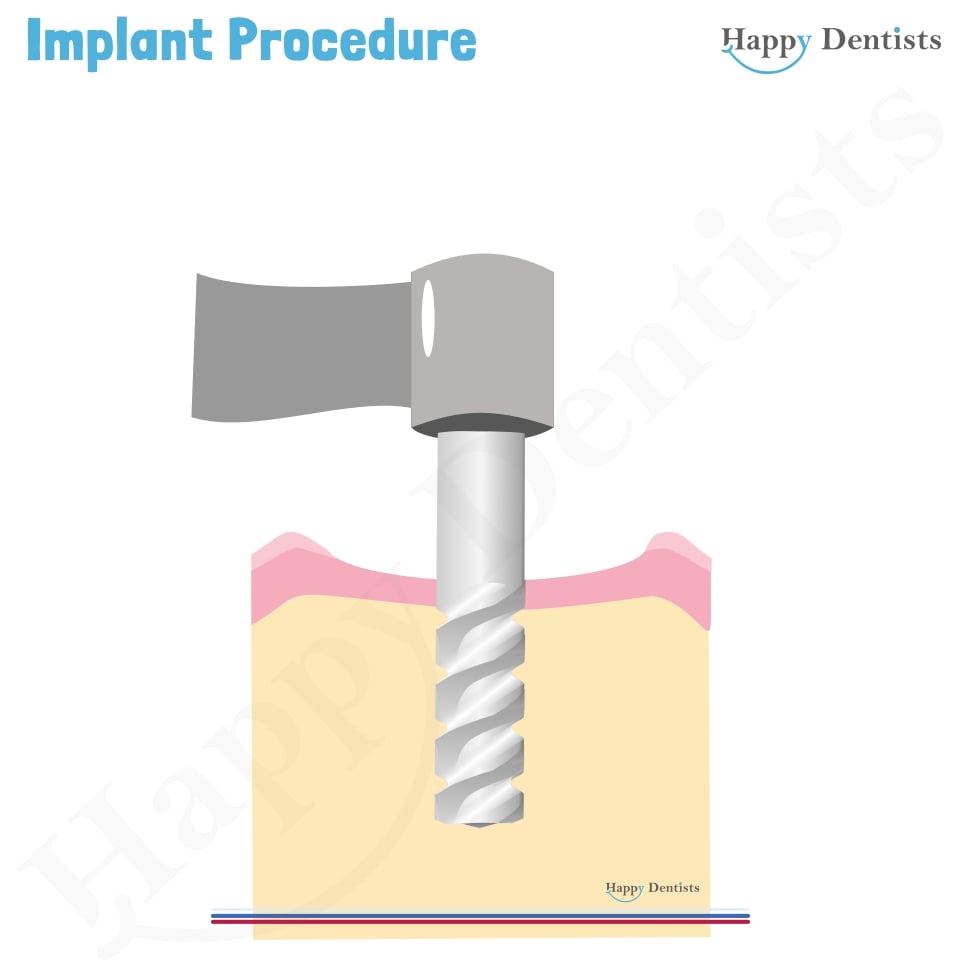
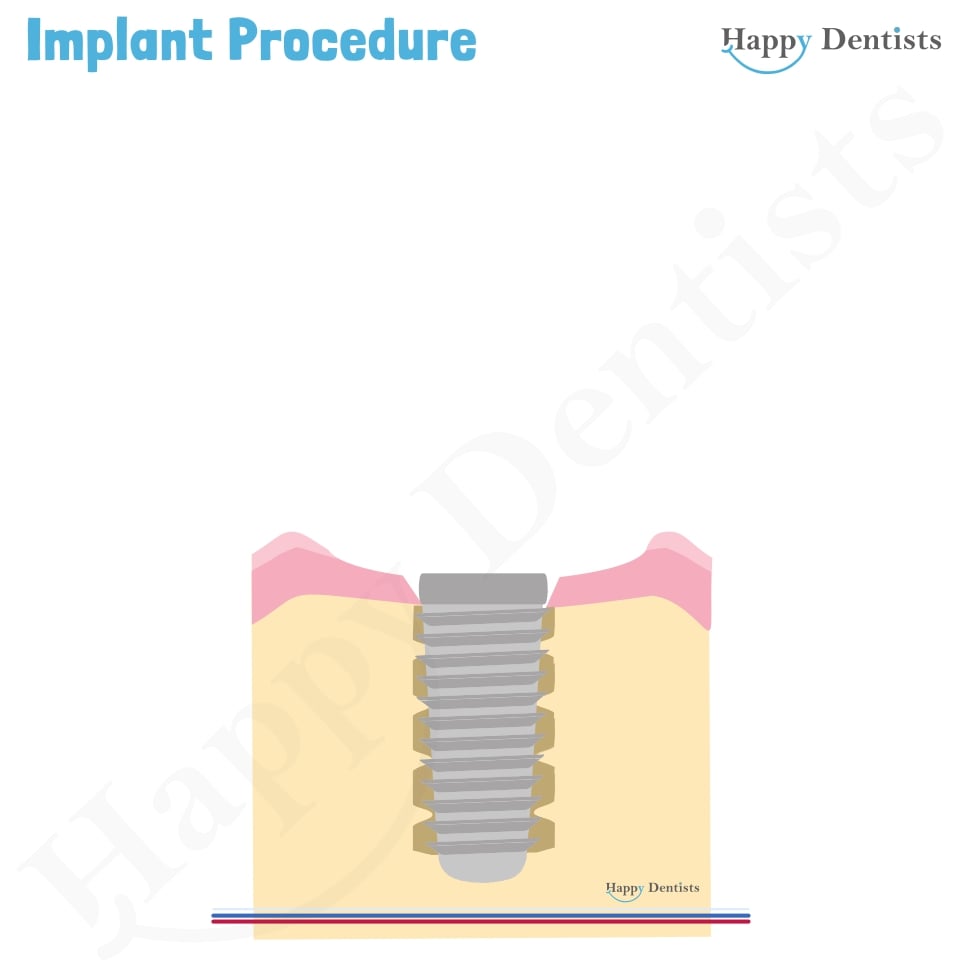
The first stage of the implant procedure involves placing the titanium screw into the bone, below the gum line. This is then stitched with dissolvable sutures which can 7-14 days to dissolve. Depending on the type of replacement option this may be one implant or a few (bridge, implant denture). Once placed, the surrounding area will be left to heal for a several months. During this time, the body will add bone right up to the implant and fuse with it. A process known as osseointegration.
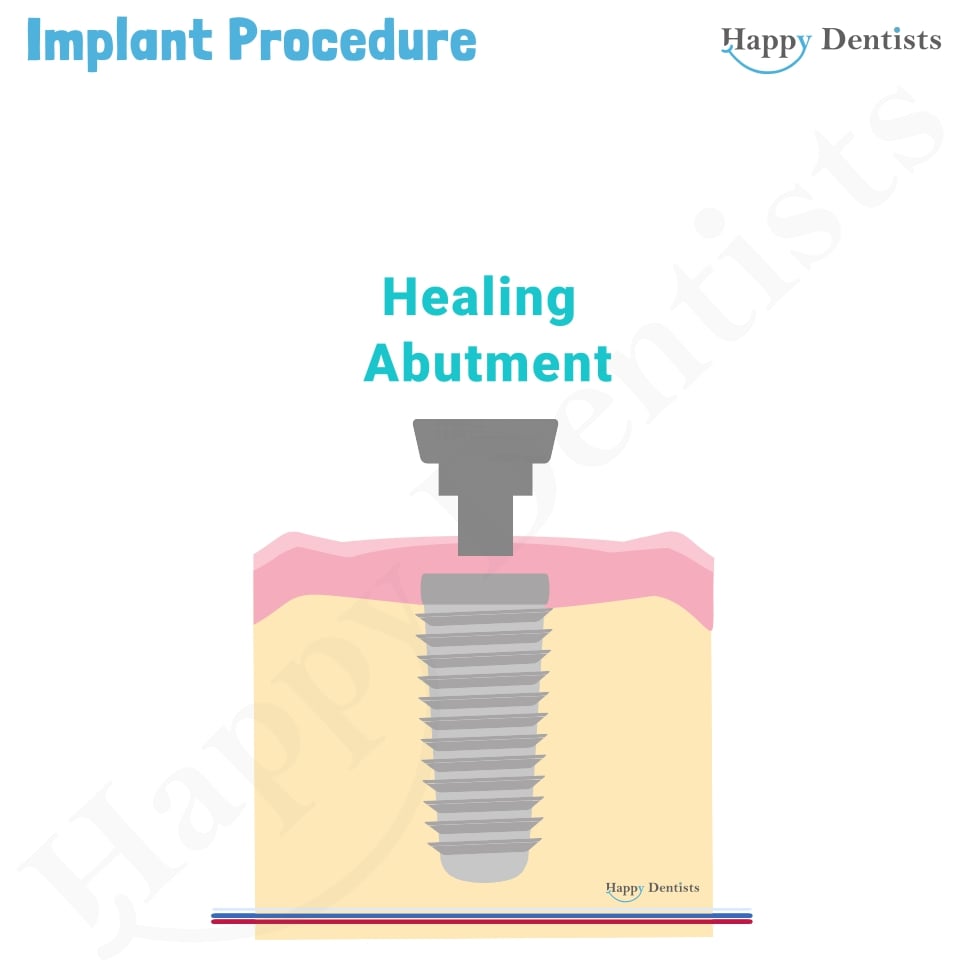
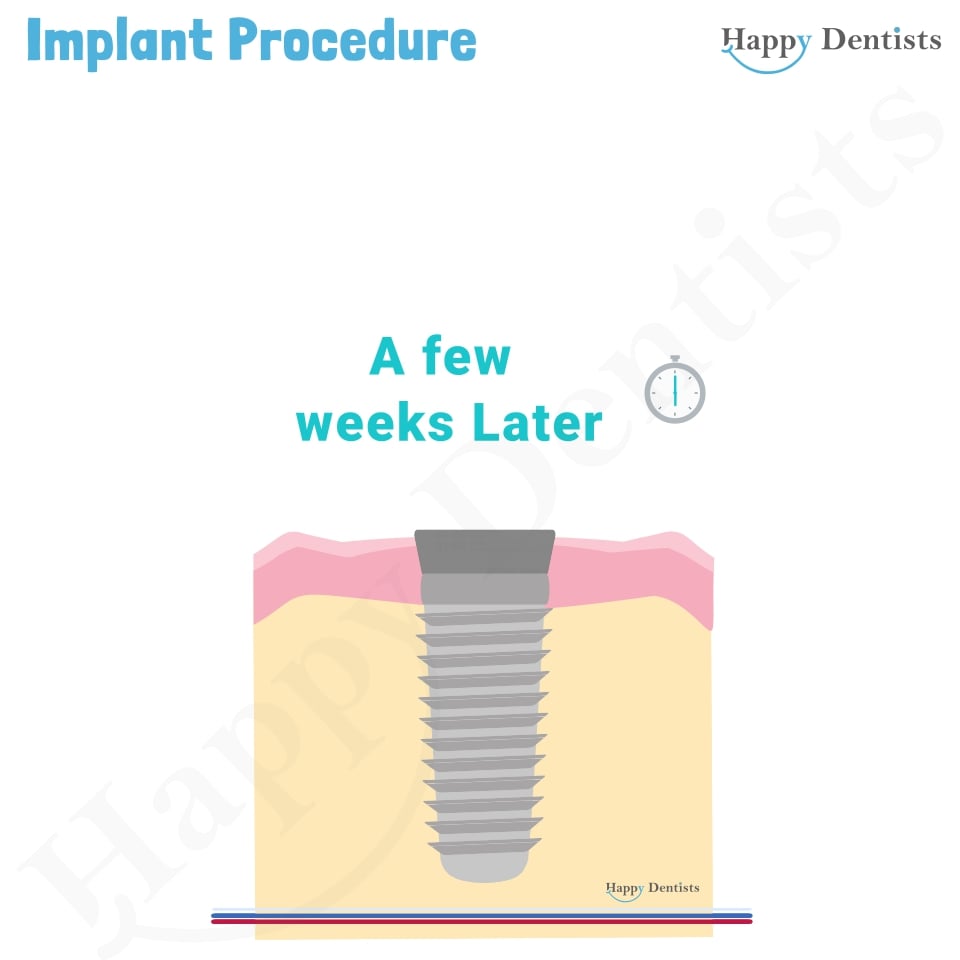
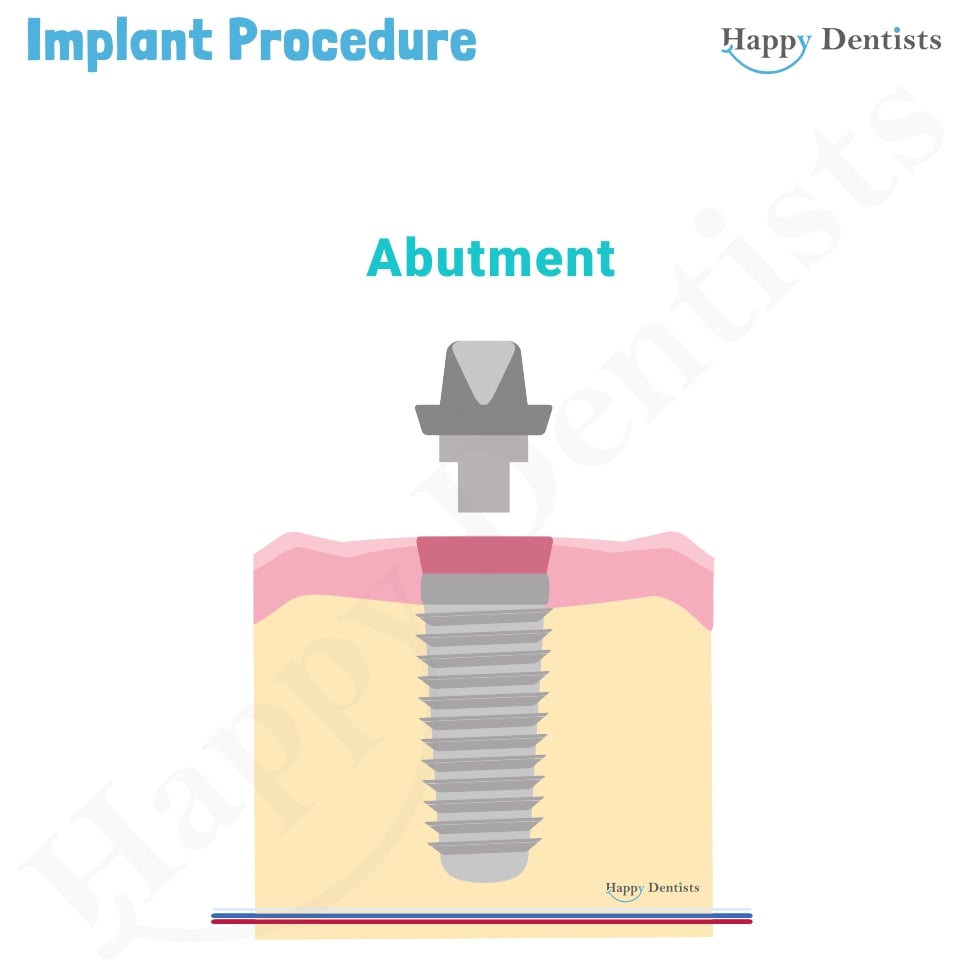
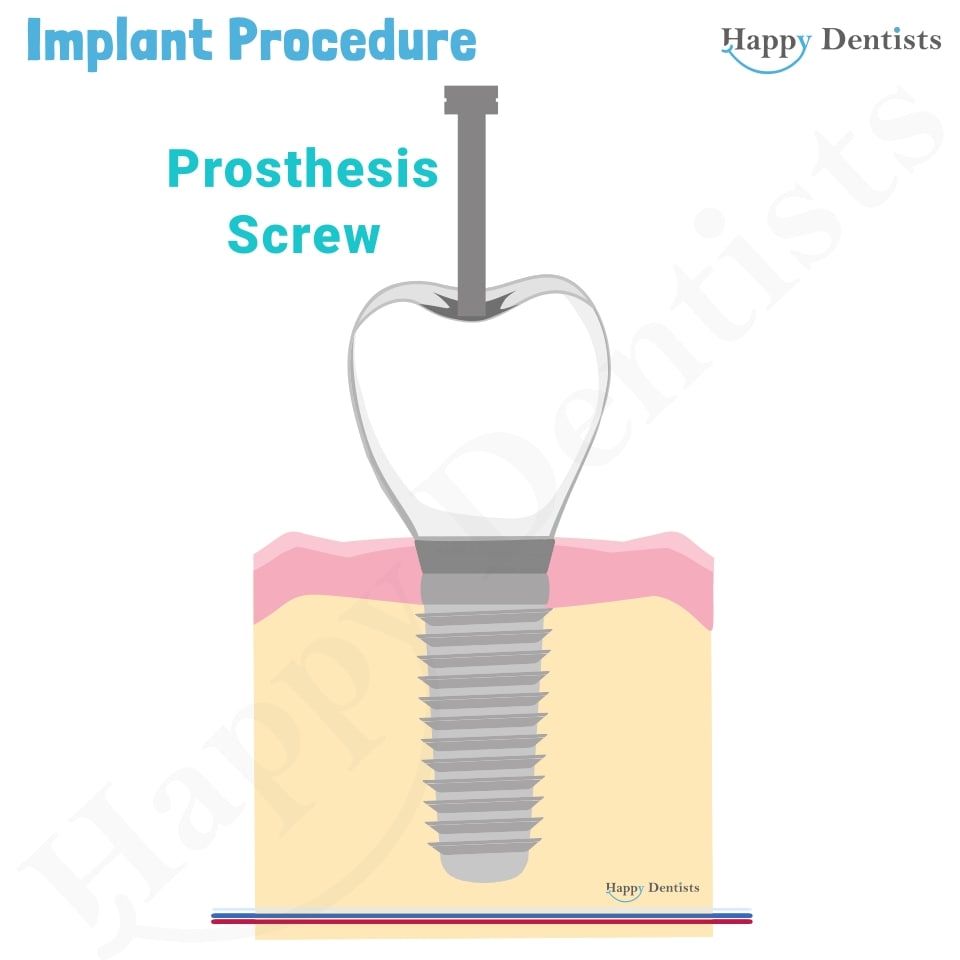
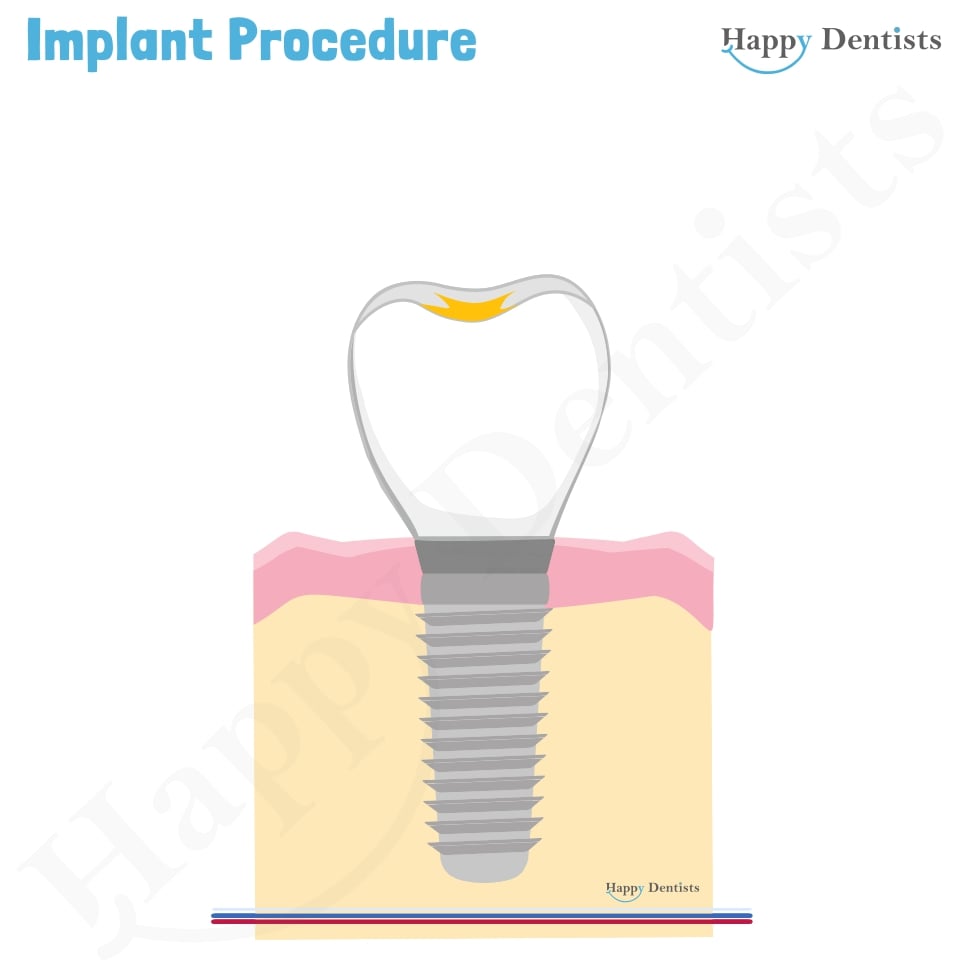
After the healing period, the implant will be surgically exposed. The implant is surgically exposed & the abutment is fitted to the implant (the screw). This is the part that will connect the implant to the crown (tooth part) later. X-rays are often taken to confirm the location and position of the abutment. Once satisfied the clinician will take an impression of your teeth & implant for the crown fabrication. Your clinician may wait a few weeks to allow the gums to shape around the abutment.
Your oral health practitioner will test the implants integration with the bone as it must be strong enough to support a denture or crown that will have to withstand chewing forces and normal function. Once satisfied they will take an impression of your teeth to fit your dental crown. This can be cemented onto the abutment or fixed to the abutment with a screw that can only be removed by your dentist.
It is important that you book and attend yearly dental reviews yearly so that continue monitoring and assessment of the implant can be done. This can help to improve the longevity of the artificial tooth.
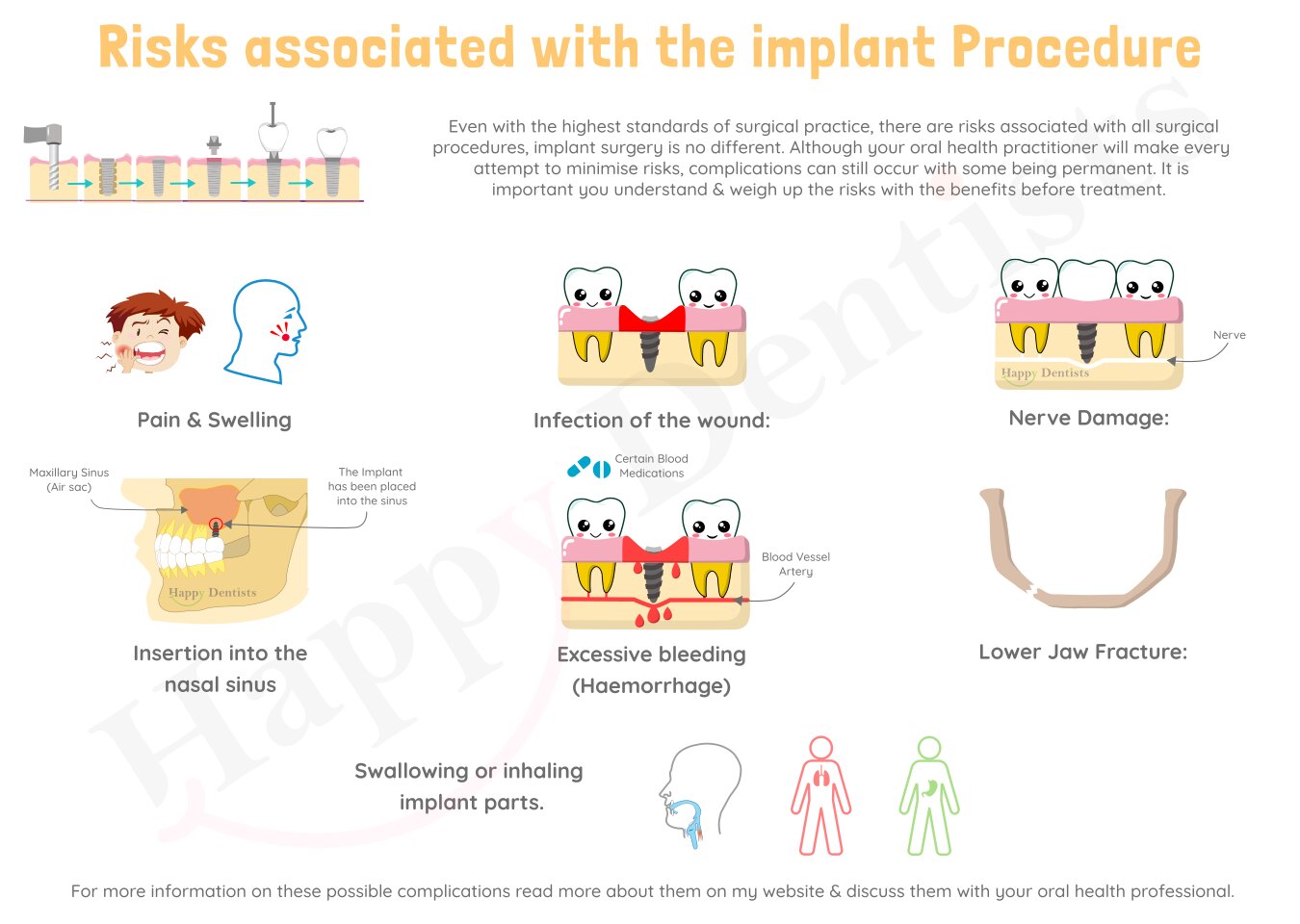
- Pain and Swelling:
- Infection of the wound:
- Swallowing or inhaling implant parts:
- Insertion into the Nasal Sinus:
- Excessive bleeding (Haemorrhage)
- Lower Jaw Fracture:
- Nerve Damage:
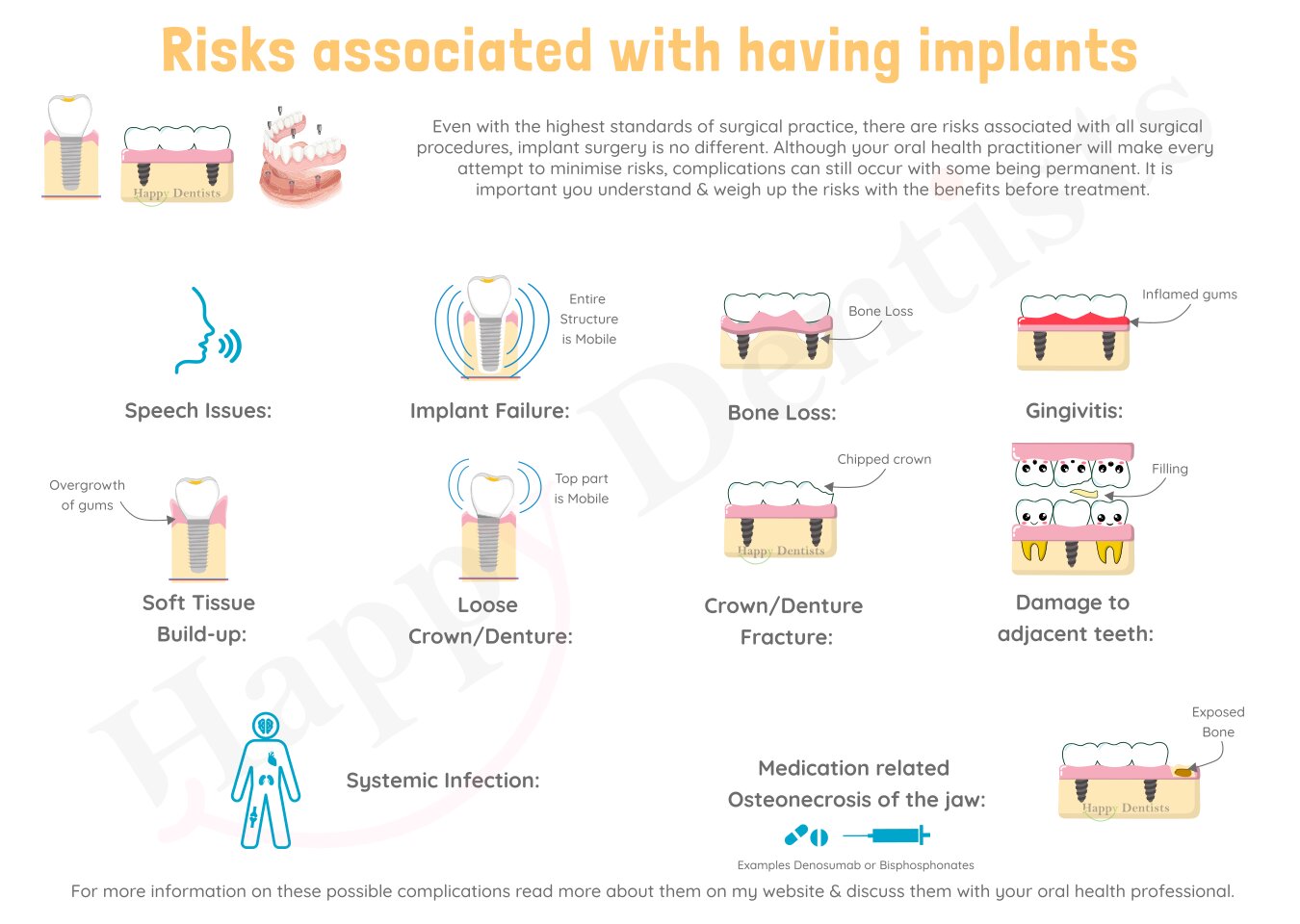
- Speech issues:
- Implant failure:
- Gingivitis:
- Bone loss:
- Soft Tissue Build-up (hyperplasia):
- Crown/Denture fracture:
- Loose prosthesis (Crown/denture):
- Damage to adjacent teeth:
- Medication related osteonecrosis of the jaw (MRONJ):
- Systemic infection:
Risks and Possible Complications:
Even with the highest standards of surgical practice, there are risks associated with all surgical procedures which makes implant surgery no different. Although your oral health practitioner will make every attempt to minimise risks, complications can still occur with some being permanent. It is important you understand and weigh up the risks with the benefits before treatment. The following possible complications are listed below to help you make an informed decision regarding the potential risks that can occur. They are not to scare you, but to help you make a well-informed decision. It is not an extensive list with all the possible complications. It is important to inform your dentist of all your medical history, medications you are taking, your occupation and any concerns to help the dentist provide a personalised risk complication information that is specific to you.
Risks during Implant Surgery
(click here to see the picture above)Pain (discomfort) and swelling can be expected and the amount of which can vary depending on the number of implants placed in the jaw. This may last for a few days. The pain and discomfort differ for everyone depending on their pain tolerance. Your oral health practitioner can prescribe pain relievers. Pain starts to decrease after the second day and continues to go down. Some people may need pain relievers for one week after. If the pain does not seem to be going down as the days go by, inform you oral health practitioner as they can help you.
An infection may occur around the implant. This may require antibiotic treatment. Serious infections usually are not related to the implants but may start after the implant has been placed. If you have fever, enduring pain around the implant or feel largely unwell inform your oral health practitioner. If an infection cannot be resolved, the dental implant may have to be taken out.
The components required for an implant are quite small and sometimes just due to poor luck they can be accidentally swallowed or inhaled. If this occurs it can go to one of two places, either you stomach where it will take time before it leaves your body by your waste system this isn’t associated with many issues, or alternatively it can go into your lungs which can have breathing obstructions. If it enters your lungs this is more of a problem and may need to be removed.
The sinuses are air-filled sacs that are connected to your nose. Implants being placed into the upper jaw may come in contact or go through the lining of the sinus within the bone (maxillary sinus), which may result in an infection (sinusitis). Antibiotics may be required to treat the infection. Rarely, excessive bleeding may be associated with the infected sinus.
In rare cases, there may be excessive bleeding from the implant site that may be life-threatening and require a blood transfusion.
Although rare, if you have a thin lower jaw due to bone loss, there is a chance that this could break during the procedure. If this occurs specialist treatment may be needed.
Sometimes implant can push against major nerves in the jaw, which can bruise them. This can result in tingling, numbness, and loss of feeling in the gums, cheeks, lips, chin, and tongue. Often this is temporary, and the nerve heals itself of the pain, tingling and numbness. The time taken for this to occur varies, it can take up to 6-18 months. In rare cases, the nerve may not heal completely, and the altered sensation may be permanent. In some cases, this may be able to be treated by a specialist. Talk to your oral health practitioner to learn more about this.
Risks associated with having Implants
(click here to see the picture above)Some patients may have altered speech after the fitting of their artificial tooth, bridge, or denture. It tends to occur more with the dentures, and usually resolves once the patient gets used to the different feel of the mouth. If not, then speech therapy may be necessary.
One or more implants may fail to successfully integrate properly with the jawbone. This can be due to multi-reasons. Your oral health practitioner may have to remove the implant and place another implant in a nearby spot in the bone. Alternatively, they may remove the failed implant and insert it in the same place once the bone has healed thoroughly.
This is inflammation of the gums without bone loss which can occur around an implant or tooth. This is a result of poor oral hygiene which can cause pain in some people. Ensure you have adequate oral hygiene (brushing and flossing) standards if concerned or unsure ask your oral health practitioner.
In some patients implant treatment may worsen the bone loss in the area the surrounding implant. Often these are patients with untreated or uncontrolled periodontitis.
In some patients the gum tissue may grow over the top of the implant where it is meant to protrude from. This can be tender, red, and unsightly. Poor oral hygiene can exacerbate this. Additional surgery may be required in these cases.
A part of the prosthesis (crown or denture) can chip or fracture. This can occur due to multiple factors including bite force, remaining teeth, eating habit and type of food just to name a few. If the fracture is serious, then a new prosthesis may have to be prepared and attached again.
Just like any screws overtime the one that is placed holding the crown or denture can become loosened. This can cause the denture or crown to feel loose. If this occurs, you should see your oral health practitioner as they will be able help you to tighten it or replace it with a new one depending on the situation.
Teeth adjacent to an implant may be adversely affected although this is quite rare, they may require root canal treatment or uncommonly removal.
Patients that take anti-bone resorbing medication such as bisphosphonates or denosumab are at an increased risk of infection and necrosis of the bone near the implant. This may result in the implant failing to integrate. It is important that you discuss all the medication that you take or have taken with your oral health practitioner.
In certain people, implants can result in infection other than the implant location. This can lead to a life-threatening infection of the heart (endocarditis). People that have had heart value surgery, have congenital heart disease, or rheumatic heart disease are most at risk of this rare complication .It is important that you inform your oral health practitioner with the all the conditions that you have been diagnosed with.
Well Done!
If you have finished reading all the information on this page, get a certificate for your hard work.
Still have concerns?
This page provides general information about dental topics. It does not contain all the known facts of this subject and is not intended to replace personal advice from your dentist. If your not sure about anything on this site, contact us or speak to your local oral health practitioner. Make sure you give your local oral health practitioner your complete medical history and dental history.
A selection of the references used:
Chen ST, Buser D. Clinical and esthetic outcomes of implants placed in postextraction sites. Int J Oral Maxillofac Implants. 2009;24 Suppl:186-217.
Esposito, M., Grusovin, M. G., Polyzos, I. P., Felice, P., & Worthington, H. V. (2010). Timing of implant placement after tooth extraction: immediate, immediate-delayed or delayed implants? A Cochrane systematic review. European journal of oral implantology, 3(3).
Esposito, M., Zucchelli, G., Cannizzaro, G., Checchi, L., Barausse, C., Trullenque-Eriksson, A., & Felice, P. (2017). Immediate, immediate-delayed (6 weeks) and delayed (4 months) post-extractive single implants: 1-year post-loading data from a randomised controlled trial. European journal of oral implantology, 10(1), 11–26.
Steigenga, J. T., Al-Shammari, K. F., Nociti, F. H., Misch, C. E., & Wang, H. L. (2003). Dental implant design and its relationship to long-term implant success. Implant dentistry, 12(4), 306-317.
Moy, P. K., Medina, D., Shetty, V., & Aghaloo, T. L. (2005). Dental implant failure rates and associated risk factors. International Journal of Oral & Maxillofacial Implants, 20(4).
Kim, S. G. (2011). Clinical complications of dental implants. Implant Dentistry—A Rapidly Evolving Practice, 2, 467-490.
Lang, N. P., Wilson, T. G., & Corbet, E. F. (2000). Biological complications with dental implants: their prevention, diagnosis and treatment Note. Clinical Oral Implants Research: Chapter 9, 11, 146-155.
Froum, S. J. (Ed.). (2015). Dental implant complications: etiology, prevention, and treatment. John Wiley & Son
Ata‐Ali, J., Ata‐Ali, F., Peñarrocha‐Oltra, D., & Galindo‐Moreno, P. (2016). What is the impact of bisphosphonate therapy upon dental implant survival? A systematic review and meta‐analysis. Clinical oral implants research, 27(2), e38-e46.
Kumar, M. N., & Honne, T. (2012). Survival of dental implants in bisphosphonate users versus non-users: a systematic review. The European journal of prosthodontics and restorative dentistry, 20(4), 159-162.
Images adapted:
Adapted from free dental picture by authority dental" (CC BY 2.0) by Authority Dental