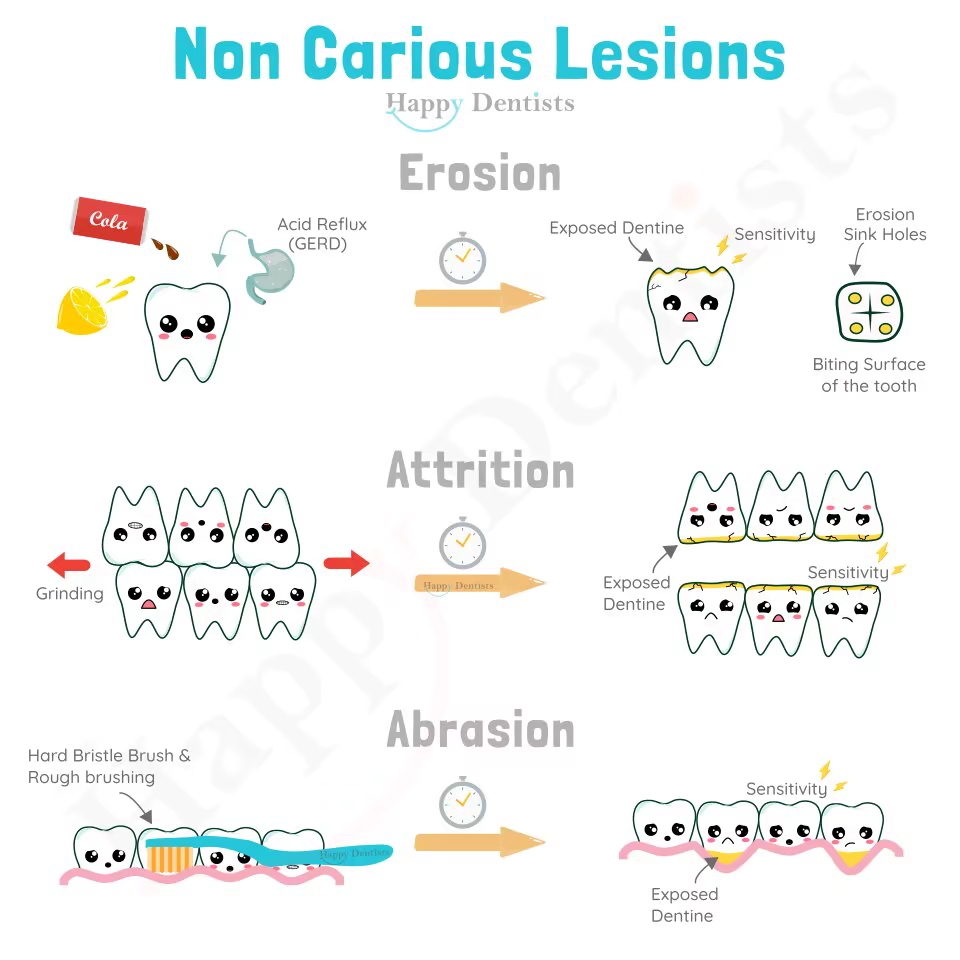
Cause of Erosion
Dental erosion is the irreversible loss of dental tissue as
a result of acid breakdown that was not involving bacterial
plaque acid.
This results not only in a clinically detectable defect, but
also softens the tooth surface, making it more prone to
abrasion and attrition. Hence why these are grouped as
non-carious lesions.
The two types of Dental erosion causes are intrinsic acid
(from inside the body) and extrinsic acid (from outside the
body).
Intrinsic acid originates from the gut and the gastric
acid. It is associated with dental erosion on the palate
surfaces of the teeth. This can be a result of the
presence of indigestion, heartburn, or epigastric pain, it
may be related to spontaneous or self-induced vomiting
associated with underlying medical conditions such as
irritable bowel syndrome or bulimia nervosa.
Extrinsic acid originates from drinks (soft drinks, fruit
juices, alcohol), foods (citrus, vinegar), medications
(vitamin C, aspirin, iron), and environment (work related
exposure). Unlike caries demineralisation, there is no
clear critical pH for erosion; other factors must be
considered such as beverage mineral content or the
chelating potential of chemicals such as citrate.
Additionally, alcohol may induce reflux, medications may
induce dry mouth or vomiting, and active lifestyles are
associated with greater risk of erosion.
How May A Dentist Diagnosis It
Clinicians use the appearance of the teeth to diagnosis as
erosion, as it has a distinct appearance and effect on
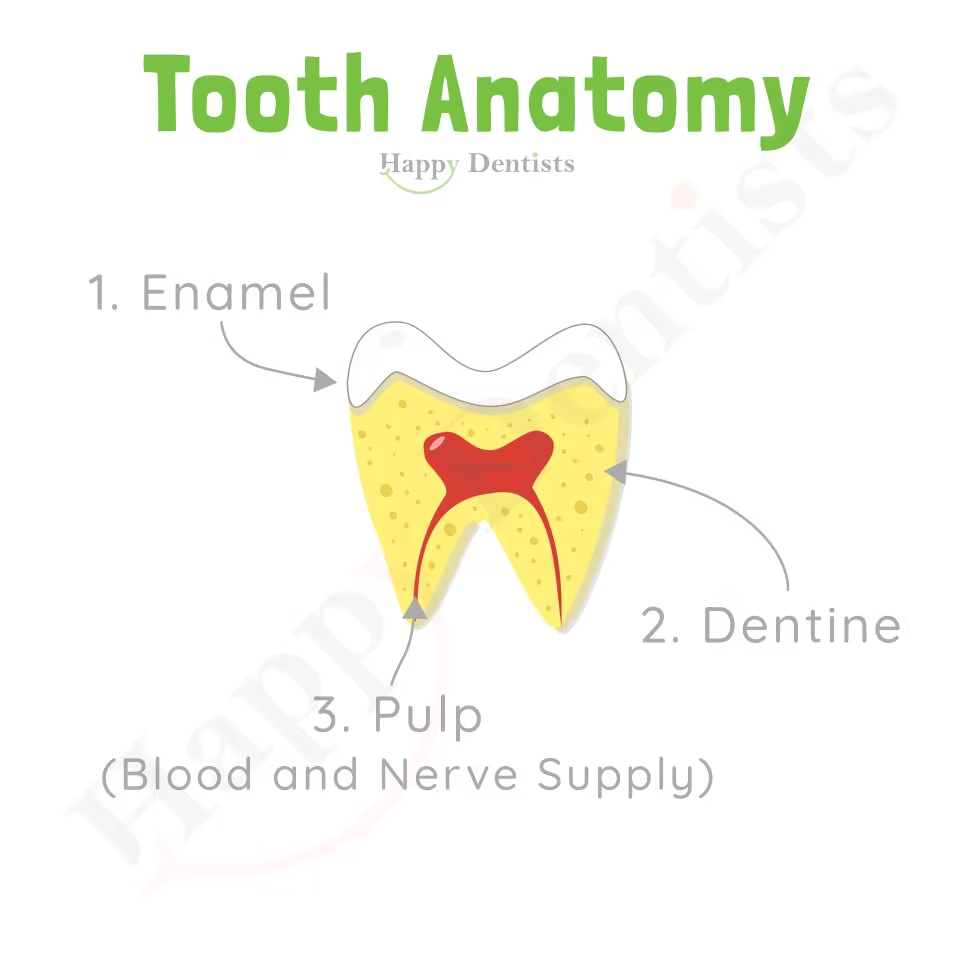
teeth. Acid thins the enamel and ledges become visible.
Cusps on teeth become cupped and fillings are more
noticeable as the tooth has eroded away. Incisal edges
become grooved, and areas of dentine become exposed. It
gives a glazed enamel surfaces, can result in dentine
hypersensitivity, and there may be a lack of plaque.
Teeth may appear darker as dentine is exposed and patients
may be concern about aesthetics once significant volume of
tooth structure has been lost. This results in shortened
teeth and dentinal exposure.
The pattern of erosion will give clues about the cause:
vomiting tends to affect the back surfaces of all the upper
teeth, reflux tends to affect the back surfaces of the upper
molar teeth, dietary liquids tend to affect the biting
surfaces of lower teeth, and dietary solids tend to affect
the biting surfaces of both upper and lower.
In saying that, a diagnosis of dental erosion is made more
difficult because of the triad of wear mechanisms and
therefore careful history taking is important let your oral
health practitioner know all about your diet and past
medical history.
How May A Dentist Manage It
The first step is usually trying to control the factors
causing the erosion if they can be identified and
controlled.
Prevention may stop progression at an early stage and should
be specific to each patient.
The erosion might be recorded and monitored with
measurements, study casts and photographs by your oral
health practitioner. A ‘wait and see’ philosophy is
generally recommended unless patients complain of pain,
sensitivity, function, or aesthetics.
Dietary analysis facilitates tailored dietary counselling.
Specifically, acidic food and drinks should be limited to
mealtimes where salivary flow and buffering quality is
highest. Sugar-free gum increases salivary flow and
encourages remineralisation. Finishing a meal with dairy
will also neutralise intra-oral acid. Acidic drinks should
be consumed with a straw placed toward the back of the mouth
avoiding swishing it around or touching the teeth. Rinsing
with water immediately after acid exposure is also very
effective.
Fluoride and desensitising agents aid remineralisation and
decrease sensitivity. Toothpaste may be applied prior to an
erosive challenge and this is preferable to brushing after
an exposure. In fact you should avoid brushing immediately
after an acid insult. Tooth Mousse (CPP-ACP) contains all
the raw products for remineralisation and is particularly
effective at low pH. Tooth Mousse may be smeared over teeth
just before bedtime in a patient with nocturnal reflux.
Sensitivity may be managed with a filling, dentine bonding
agents (which may last up to 3 months), fissure sealants
(which may last up to 9 months). However, these do not last
forever, and some commit you to the restoration cycle.
Cause of Attrition
Attrition is wearing of the tooth surface which occurs from
tooth-to-tooth contact. It occurs from grinding which is
commonly associated with stress
The prevalence of grinding varies considerably in the
literature. It appears that everyone grinds to some degree
depending on life events; however, if this behaviour becomes
excessive, the wear rate may become excessive for a person’s
age.
Factors that accelerate loss of tooth tissue include MDMA,
SSRIs, and habitual chewing on hard foods. It is not clear
whether lack of posterior support contributes.
How May A Dentist Diagnosis It
Clinicians use the appearance of the teeth to diagnosis
attrition, as it has a distinct appearance and effect on
teeth.
Grinding commonly creates facets, described as a relatively
flat area with a well-circumscribed border. Matching facets
typically appear on both opposing teeth.
If attrition is the predominantly active mechanism of tooth
wear, the exposed dentine remains flat without evidence of
scooping (which would be observed in erosion or cases
superimposed with erosion).
In severe cases, grinding causes enamel flaking and cusp
fractures. Symptoms of TMD, overworked muscles of
mastication or awareness of tooth grinding can suggest
active attrition.
How May A Dentist Manage It
Stress management or referral for professional assessment
may be appropriate in some circumstances.
An occlusal splint will prevent opposing tooth contacts and
reduce the wear rate. It will work like a phone case in that
you break the splint rather than your teeth. It can also
help relief pressure on the jaw joint in certain situations.
Tooth Mousse can help to reduced wear when used as a
lubricant over occlusal surfaces during simulated grinding
although this has only been demonstrated in vitro studies.
Restorative appliances and techniques may help to create
restorative space and try to rebuild the teeth to a
reasonable height if they have been worn away. Speak to your
oral health practitioner about this as you may require
referral to a specialist.
Cause of Abrasion
Attrition is wearing of the tooth surface which occurs by
friction of external material. Typically, specific tooth
surfaces are affected depending on the precise cause.
Abrasion may result from: habitually eating hard foods such
as nuts and seeds, occupational habits such as holding
hairpins between the incisors, or toothbrushing.
How May A Dentist Diagnosis It
Clinicians use the appearance of the teeth to diagnosis
abrasion, as it has a distinct appearance and effect on
teeth.
Abrasion from occupational habits and hard foods is often
identified by asymmetric wear in the form of a ‘notch’ on
the anterior teeth. A history of a continuing habit, such as
pipe usage, indicates activity.
A wedge-shaped non-carious cervical lesion is a strong
indicator of toothbrush or dentifrice abrasion although
superimposed erosion may be a significant contributor.
How May A Dentist Manage It
A careful history is required to identify abrasive factors.
Therefore, it is important you tell your dentist all about
your habits including brushing, smoking and tooth biting.
You must be made aware of the problem so that you can take
responsibility for the prevention of further wear. The use
of an electric toothbrush with sensors can help reduce
abrasion phenomena especially if damage is associated to the
pressure.